Shin Splints
 ‘Shin splints’ tends to be a general term often used to describe any pain that is felt along the shin bone, particularly during exercise. Technically speaking, there are three conditions that tend to fall under the category of shin splints, which are:
‘Shin splints’ tends to be a general term often used to describe any pain that is felt along the shin bone, particularly during exercise. Technically speaking, there are three conditions that tend to fall under the category of shin splints, which are:
- Medial tibial stress syndrome
- Anterior compartment syndrome
- Tibial stress fracture
We’re going to be talking about the most common cause of shin splints – medial tibial stress syndrome – but here is a quick look at the other two causes:
Anterior compartment syndrome
Your lower leg is made up of four compartments. Each compartment houses specific muscles, tissues, nerves and arteries, and is enclosed by a lining tissue that prevents the compartment from over-expanding.
When one or more muscles within the anterior compartment are overused, it swells, resulting in a tight (and often painful) feeling at the front of the shins. This pressure and discomfort can settle with rest, and recur when you start exercising again.
Tibial stress fracture
Tibial stress fractures occur when excess and repetitive stress on the shin bone results in a fracture starting to form. Stress fractures start as small cracks which may have no painful symptoms or a dull ache or niggle. Without treatment, and with ongoing stress on the bone, the fracture worsens and becomes more painful. As stress fractures can take many weeks to show up on x-rays, this may explain why it is initially diagnosed as a broader ‘shin splints’ instead.
Medial tibial stress syndrome
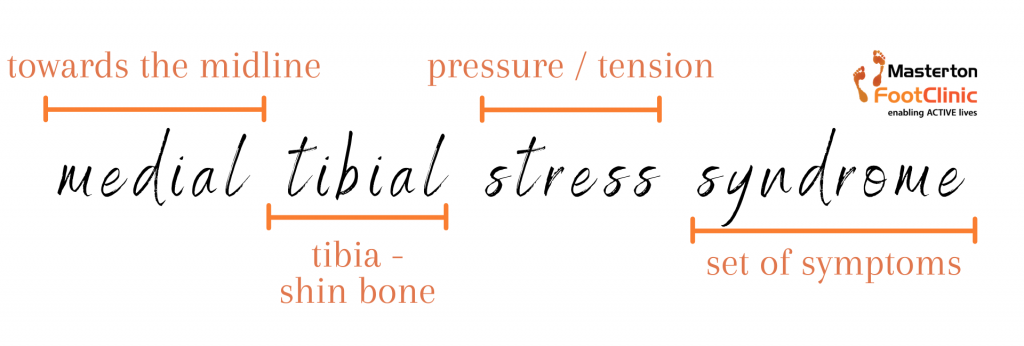
Like the name indicates, medial tibial stress syndrome is caused by excess stress on the inside border of the tibia (shin bone).
The stress may affect the tendons and muscles that attach to the shin bone, or from the lining of the shin bone itself. This causes pain and swelling, making it painful to continue movements that activate the muscles at the front and inside of the shins, which are often involved in activities like running.
MTSS causes & symptoms
Any activities or factors that contribute to increased stress on the tibia can result in MTSS. This includes:
- Physical activity – starting new physical activities or increasing the intensity or duration of existing activities
- Biomechanical factors – your foot posture, like flat fleet, and lower limb biomechanical function can contribute to the onset of MTSS
- Other factors – like exercising with unsupportive or worn-out shoes
Aside from pain at the front and inside of the shins, you may experience some swelling, and your symptoms may be aggravated by exercise.
Treating MTSS shin splints
Treating shin splints starts with relieving your initial symptoms, understanding what has caused them (and so may continue to stress the shins) so that the right environment can be created to allow the damaged structures to heal, and then put the right measures in place to help prevent shin splints from becoming an ongoing problem in the future. To do this, we may use one or a combination of:
- 3D-scanned custom foot orthotics
- Strapping, splinting or bracing
- Footwear adjustment to more stabilising and supportive shoes
- A stretching and strengthening programme
- Gait retraining following a running assessment
Using RICE (rest, ice, compression and elevation) can help settle your initial painful symptoms.
FAQs
I never used to get shin splints but I think I am now, what has changed?
This is an important question that we investigate as part of your assessment. It could be related to changes in footwear, it could be linked to your foot type and excessively loading the feet through involvement in certain sports or activities, it could be linked to areas where muscles have grown tight or weak, it could be related to previous injuries like ankle sprains that have left you less stable than you were before – you name it. We’ll explore all of these options and more at your appointment to find the cause of your shin splints so we can direct your treatment appropriately.
Can I prevent shin splints?
You can definitely reduce the risk – and this starts with understanding what has caused your current case of shin splints so we can address these factors and help prevent them from interfering in the future. We’ll also look at general risk factors that can lead to you overloading your shins and muscles more than you need to, and help optimise this function too.
Can children get shin splints?
Yes, children can and do definitely get shin splints. There’s also another condition called Osgood Schlatters which describes growing pains in the knees, which presents as pain just below the kneecap. This is why it’s always a good idea to see a podiatrist who can accurately diagnose the problem and prescribe the right treatment plan for your child.
What do shin splints feel like?
Shin splints feel like pain or tenderness at the front (and often insides) of the shin bone. Your pain may feel worse at the start of exercise or halfway through, then reduce as you continue to exercise or rest. If you feel notable pressure or tightness in your shins, it’s important to check for compartment syndrome. If your pain does not settle after some rest or lingers to the following days, a stress fracture should be investigated.
What can I do at home to help reduce the risk of shin splints?
You can reduce your risk of shin splints by warming up before exercise – particularly by stretching the calves and hamstrings well. If you’re getting into a new sport (or exercise altogether), ensure you gradually increase the amount of exercise that you are doing, instead of going too hard too fast, as this increases your risk of shin splints alongside various other injuries. You can also add lower limb strengthening to your exercise routine, including your hips, knee, feet and legs. Make sure you’re wearing good, supportive shoes every time you exercise. Finally, if you feel aches and niggles during exercise, see your podiatrist early – before it progresses to a full-blown injury like shin splints.


